COVID-19: End of April Update

May 5, 2020
My 25th reunion for medical school was held on Zoom on April 25th. Two classmates were recovering from COVID-19, neither of whom had a severe case. For people our age, recovery without issue is not uncommon. And the more we learn about the virus, the more thoughtful we can be in planning for the future.
A few patients have mentioned a recent viral video of two California doctors in Bakersfield, California urging Governor Newsom to open the economy. You are welcome to watch it, but it has received quick rebuke from many, including me. There is a lot of misinformation in what they say. That being said, if physicians are ill informed, perhaps it’s important we review some of the data that’s out there and update on a few key points. As you all know, our goal is to keep you safe!
1. Flattening of the curve: Here we are in week six or seven of the stay at home order. Is it working? Yes! It was on March 17 that I sent an email/posted a blog about flattening the curve and talked about social distancing. Seems like a lifetime ago. The goal was to stay at home, prevent the exponential spread of the illness so our communities could handle those that were sick or going to become sick. You’re doing it! Because of your efforts, in the Chicago area we are using the McCormick Place temporary hospital less. We have not had to ration care in Illinois like they have had to do in Italy. Many lives have been lost, sadly, but as a community we are doing well. It may be that the stay at home order in Illinois gets lifted sooner than the end of May. We need 14 days of declining numbers, though, and we’re not declining yet. Keep it up!
2. Did we go overboard? Folks can look at empty beds and available ventilators in ICUs and at McCormick place and say, “Was there a better way? Could we have protected lives AND not killed the economy?” A good article if you want to nerd out a bit on statistics said this, “[A]pocalyptic prophecies can galvanize people into action. Unfortunately, if that action works, it makes the model look as if it was wrong from the start. The only way these mathematical oracles can be truly valuable is to goose people into doing the work to ensure the predictions don’t come true—at which point it’s awfully difficult to take any credit.” Was it worth it? We can look at the approach of two different Scandinavian countries for some guidance. Sweden has not done aggressive stay-at-home efforts while Norway has. If you look closely, both countries had their first cases on about the same day at the end of February. On the logarithmic curve for the two countries on the Johns Hopkins website, you will see clearly that Norway “flattened the curve” a month ago while Sweden has yet to do so. Sweden is having a worse time of it without a shelter in place order. If we hadn’t taken these efforts, as a country we’d be much worse off.
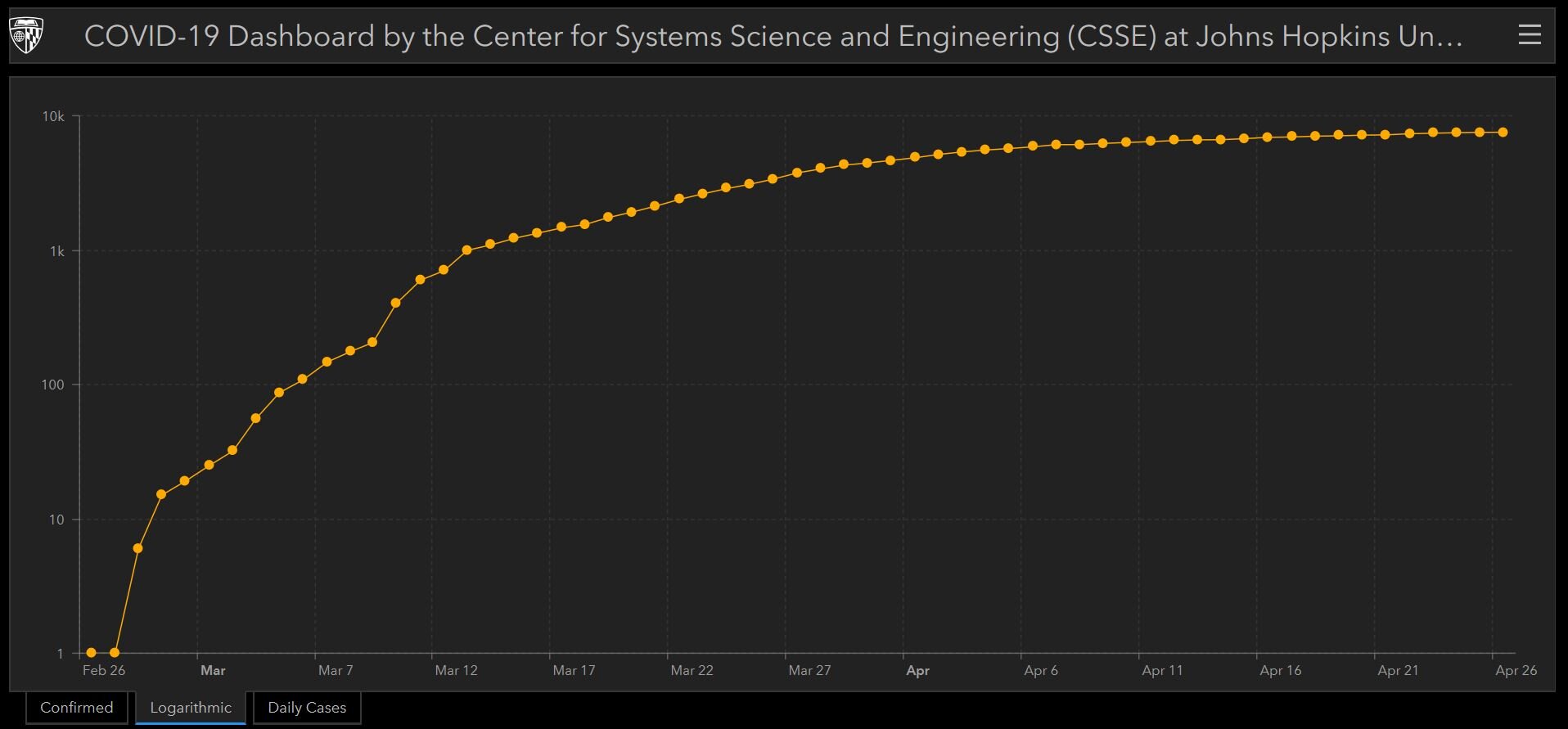
Norway has flattened the curve with strong social distancing efforts.
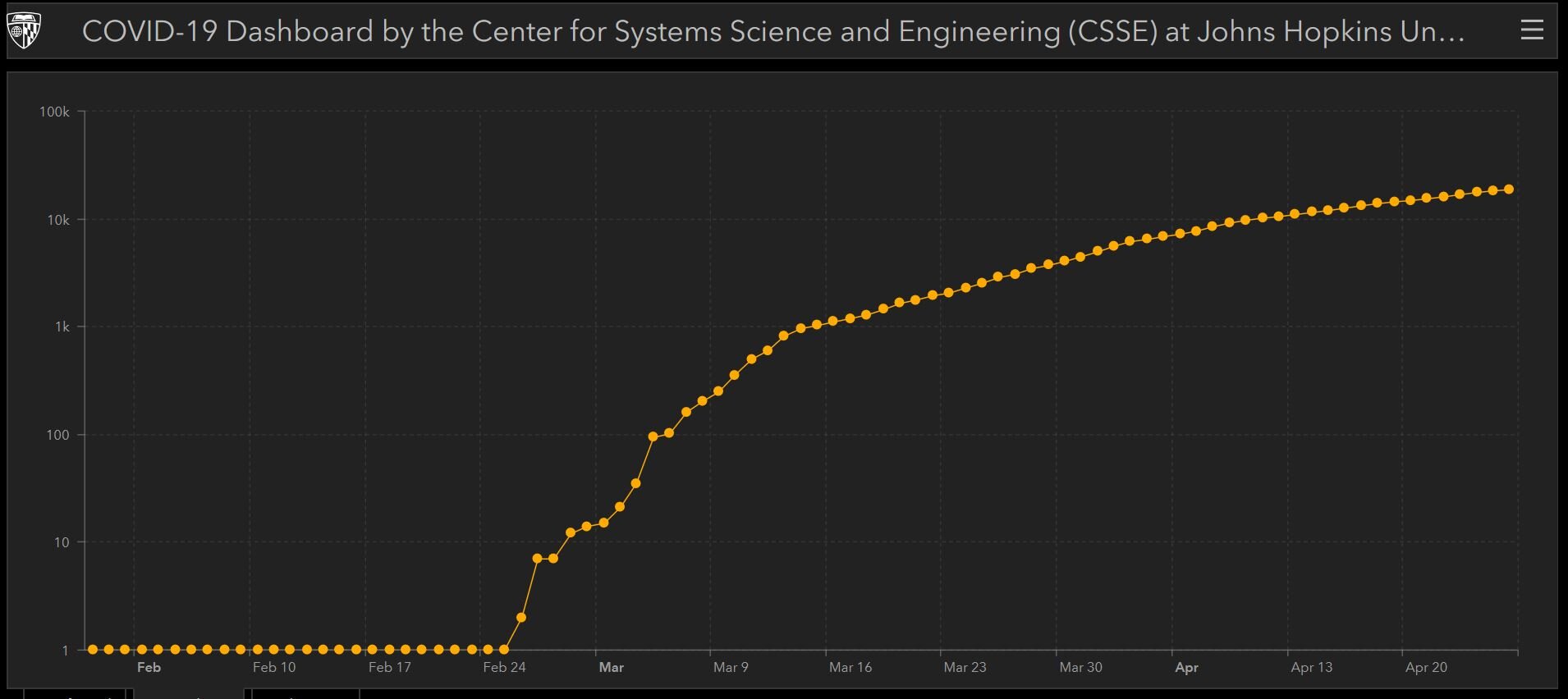
Sweden has yet to flatten the curve.
3. What about individual communities now? Champaign, IL is different than Chicago, IL. Poughkeepsie, NY is different than Manhattan, NYC. Are the same interventions needed in these different localities now? We’re learning more about this. Early on the predictive models were relying on a moving target of data and applying that data to all communities equally. We had to. Now that we have a bit more knowledge we can say more. Not all communities were hit as hard, for sure. Here’s another nerdy summary of how to use local data to make decisions about releasing from the lock down. If we have quality testing in place and good testing data to assess the disease prevalence in local communities, we can figure out how many new infections a local health system can handle without reaching its limit. If the cases have declined and reached an acceptable number, we can relax some restrictions, but if the number starts rising to an unacceptable level for the local community, “the restrictions must be…reapplied, and lifted and reapplied, as long as it takes for the population at large to build up enough immunity to the virus.”
Surveillance testing and analysis of these data is key. “Trying to see our way through the pandemic with this ‘suppress and lift’ approach is much like driving a car on a long and tortuous road, according to the author. One needs to hit the brakes and release them, again and again, to keep moving forward without crashing, all with an eye toward safely reaching one’s final destination.” This is one method for how we can use the testing data, but we’ll have to see how it gets implemented.
4. Have more people been exposed? Have I been exposed and recovered? For those of you who have been sheltering at home the chances of you having gotten COVID-19 in the past few weeks are low. In the past six weeks you haven’t had much contact with people outside your six-foot-zone-of-safety and when you’ve gone to the store, you’ve been mindful of protecting yourself with a mask and clean hands. This is good.
Could it be that an illness back in February or early March was COVID? Could you have had a mild case and recovered? What we've learned in the past month or two is that COVID-19 can present in more than one way. Initially we thought it was just a fever, cough and shortness of breath. The CDC has updated it's website to reflect this knowledge: yes fever, cough and shortness of breath are the most common, but sore throat, loss of smell, and others have been added. It's still not a complete list of ALL of the symptoms that have been associated with COVID-19. I've heard of rashes, hives, diarrhea, even potentially an increased rate of stroke. There's a self-check tool on the website, "Are my symptoms consistent with COVID-19?" Instead of using the self-check, though, reach out to your provider.
It is possible, though unlikely, that a mild illness you had in early March was COVID-19. How would you know? This is the role for antibody testing. These tests are immunoassays that look for the presence of antibodies, your immune system's response to infection. The presence of antibodies reflect potential prior infection and potential immunity to SARS-CoV-2.
Harper Health has tests from two different vendors with accuracy that is still being determined. Quest and LabCorp have recently started performing this testing, as well, but it is not clear how accurate their tests are. We're not 100% sure which vendors Quest and LabCorp are using. The accuracy of these antibody tests is an ongoing area of study.
The result for any of these tests is either a thumbs up or thumbs down with regard to prior exposure to this coronavirus (or potentially one of four others). A more detailed test, specific to SARS-CoV-2, is on the horizon.
Should you get a test? Without a known contact with a COVID-19 sufferer or a suspected illness, I'll tell you it’s very unlikely you have antibodies and protection. Most of our tests have been negative so far.
Where can you get the test? A patient of ours just went to Quest without a prescription to get antibody testing done. Click here if you want to get screened and tested at one of their draw facilities.
If you would prefer to come to one of our offices to have your blood drawn for the test, we can do that, as long as you are at least 21 days out from any symptoms from a prior infection. In an effort to keep our practice locations safe, our rules are more stringent than others’. Reach out to Priscilla and let us know if you want to come here. We are only testing members of the practice.
Keep in mind, the presence of antibodies does not prove that you are immune to SARS-CoV-2 and can’t get COVID-19 again. It’s likely, but we don’t have the research yet to prove that. I suspect that the few of you who have had illness will be protected from re-infection, though that protection may wane over time, necessitating a booster with a future vaccine. More research is coming out, literally, on a daily basis.
For the majority of you who have not had illness, we are grateful! While there are many reports of folks who have had mild illness, I can tell you first hand the severe downside of the illness. One Harper Health member nearly died in the ICU on a ventilator. He is our miracle, and will be going home at the end of the week. Another patient of mine I have known for 20 years died last week of a heart attack. While she had multiple other medical problems, she also had COVID-19 when she died. It is not a coincidence that she had COVID-19; I believe it’s the reason she had her heart attack. It was not her time to go. I will miss her greatly.
So, we want you all to avoid getting COVID-19 until a vaccine is available. When the time comes in the next few weeks and with both the data and your best interest in mind, we at Harper Health will give you OUR suggestions on how to keep you safe as you emerge from this quarantine.
We have only had a few cases of COVID-19 in the practice and the credit goes to YOU. The more you stick to it, the more you continue to be patient while at home, the lower the chance you have of getting this deadly illness. We want to keep you safe and our COVID-19 numbers low!
More to come,
Dr. Will
Sign up below to join our newsletter