COVID-19: End of October Update

Dec 8, 2020

I have to admit, the Harper Health team felt a bit under siege this week. We’ve been trying hard to stay safe and COVID-free, but there were a couple of close calls. Dr. Will had a patient in the office for his preventive physical who three days later began having symptoms that were later diagnosed as COVID. Dr. Meg examined a patient in the office with a curious symptom that ended up being her COVID presentation. In addition to these close calls, Dr. Meg heard of a “COVID Party” where a couple known to have COVID was inviting friends over to get infected so they didn’t have to worry about it over the holidays. As you can imagine, these have made us feel a little jumpy.
Why? You might say, “Your staff is almost all young. What’s the big deal?” This disease has only been around for 10 months. There’s so much we still don’t know. A certain percentage of kids get MIS-C (mult-inflammatory syndrome in children). If we get infected could we spread it to yours or mine? We don’t yet know how to identify those kids at risk. There’s also MIS-A in adults. Same deal: we don’t know yet who the population of folks are who are at risk for this. Notwithstanding, I have one patient who has died. It wasn’t her time. Another patient in his 40s with no prior risk factors who has chronic lung issues after COVID. I don’t want any of you to get COVID because I can’t predict what’s going to happen to you nor as your primary care doctors can we yet provide you any direct treatments.
We’re eight months into the pandemic and I understand there can be some COVID-fatigue. It is frustrating for those who have been doing everything right to hear infections and restrictions going up. “What else can I do?” If this were just an issue of your own personal behavior, such as exercise or eating healthy, I would fine tune your plan to make it work. The issue here is that we’re relying on our neighbors to also do the right thing. What more can you do? Well, if you hear about COVID parties, call the hosts out. If you are feeling even a bit sick, don’t leave your house. A lack of fever isn’t enough to give you license. Please stay home. And before coming to our office please tell us if you’re having any symptoms or have had any exposure to people with COVID symptoms. Be thoughtful as you fill out the pre-visit survey.
Here are some questions that I’ve heard asked and will answer in the context of now: End-of-October 2020.
Is the rate of infection really rising or is it an artifact of more testing?
It’s an important question. If you test more people then, yes, you may pick up more of the mild cases that may not have been brought to the attention of health care providers. As you can see from the graph below, the number of tests done in the US has gone up progressively since the pandemic started (orange bars). This is good! If we test more, theoretically we can identify cases and then do contact tracing to isolate the patient and prevent a serious cluster form forming. One big issue, if the goal is still to limit the spread of illness, you need to have a low enough number of cases that you can track and trace. If the case count gets too high, it can overwhelm the system. That’s what is happening now. Not only are we testing more, but a higher percentage of those tests are also turning positive (blue line). The goal here is to keep the test-positivity rate below 5%, and it’s climbing near 9%. This is worrisome.
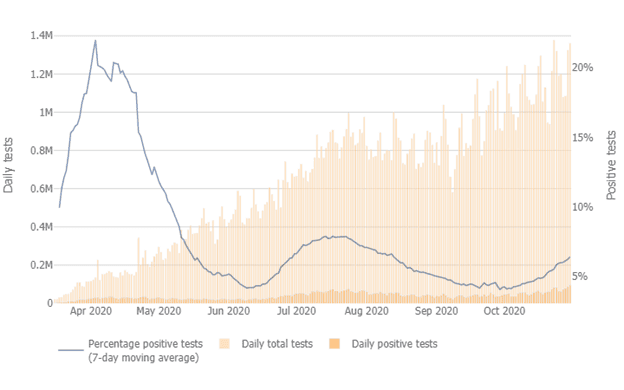
It is true that we must be cautious as we interpret the reported positivity rate in communities. States should be filtering the data so cases aren’t double counted. With the increased prevalence of the in-office rapid tests, we are seeing more positive tests at the point of care. Some of those tests get confirmed with a lab rtPCR test. If both are reported as positive then the case rate will seem higher than it really is. From the Hopkins COVID project: “When states report the number of COVID-19 tests performed, this should include the number of viral tests performed and the number of patients for which these tests were performed. Currently, states may not be distinguishing overall tests administered from the number of individuals who have been tested. This is an important limitation to the data that is available to track testing in the U.S., and states should work to address it.” As of October 14 Illinois started counting antigen tests in its total, but it's not clear whether the State is eliminating the double count. That being said, the increase in cases and hospitalizations started before this change.
Are all cases serious?
Another good question! As I have written before, there are leading indicators and lagging indicators. The leading indicator is the test positive rate. Hospitalizations and deaths come later, lagging indicators. We’ve already seen an uptick in one of the lagging indicators, hospitalizations. The trend on deaths in Illinois is going up as well.
Why is this important? First, it’s a hospital capacity issue, as it was at the beginning of the pandemic. If cases rise too fast, hospital capacity gets maxed out. This has been seen recently in areas such as El Paso and up in Green Bay. Whether you’re in a small town or big, this could become an issue fast. You don’t want to be sick and hear that there’s no room at the inn, or your room is in a tent outside. The statistics here show what’s going on in Chicago (Region 11) on the left (first) and DuPage County (Region 8) on the right (second): Cases rising. Hospitalizations rising. Available hospital and ICU beds dropping.

I want to mention something else. There is still a lot we don’t know about the long-term effects of having COVID-19. At Harper Health we don’t have a large practice, 500 patients at max. One of those patients has died and one has a serious lung issue. I don’t like those numbers, and neither should you.
I can’t say it enough; this is not just the flu.
I hear the death rate is declining. If so, should we still worry?
It is true that doctors have done a better job treating hospitalized patients, and the illness is now infecting a more resilient population. At the beginning, 25% of people admitted to the hospital for COVID-19 died. Now the rate is down to about 8%. So, yes, you’re less likely to die, but 8% is still too high for me!
It’s also true that until we have a safe and effective vaccine that enough people take, COVID-19 will be a significant problem. And since it will be, we will have complications and deaths from it. From a public health and ethical perspective, though, how many deaths are too many? To me, at this point in the pandemic, the number of total deaths per day should be declining day by day. If it’s going up, we’re not doing something right as a community. As you can see from this graph for Illinois, the trend is upward on deaths per day.

What’s the update on the vaccine?
There hasn’t been much movement in the past month. Go here if you want to read our summary of the vaccines in development. There are some vaccines trials that had been suspended for a while—the Oxford/Astra Zeneca, Johnson and Johnson, and Pfizer—but they’re back recruiting patients and finishing their Phase 3 trials. As more info comes available, I will update you.
Any new treatments on the horizon?
One drug class that I want to update you on is the antibody treatment being studied by both Eli Lilly (LY-CoV555, also known as bamlanivimab) and Regeneron (REGN-COV2). This is one of the medications that the President took when he was sick, where antibodies against the SARS-CoV2 virus made in the lab were infused in the hopes that they would bind to virus and aid in its destruction. The drug is being studied in mild to moderate illness and hospitalized patients. Eli Lilly halted its trial of the drug in hospitalized patients because of no benefit to the patients. It is still being studied in mild/moderately ill patients. Regeneron is still studying both patient populations. Neither drug has received approval from the FDA to be used in patients outside a clinical trial (except if you’re the POTUS).
Another drug to keep in mind is Vitamin D. Way back at the beginning we talked about using Vitamin D to help support your immune system. That seems to have been borne out in the data. A recent study from Spain found that 80% of patients admitted to the hospital had low Vitamin D levels. This doesn’t provide proof that a normal Vitamin D level protects you, but it is suggestive.
So, as we continue into the Fall and Winter, the virus is going to accelerate. Dry air, indoors more, COVID fatigue are all factors that will promote its spread. A patient of mine mentioned that my last post seemed a bit hopeful. As we finish October, I am less so. Please be safe: Wear a mask. Keep a physical distance. Wash your hands. Limit your exposures.
Sign up below to join our newsletter