COVID-19: Peeking around the corner

May 27, 2020
Sorry for the week off in the letter. As all states in the US are in some phase of the re-opening process, we’re getting a lot of questions about what people can do. Illinois is on the verge of moving to Phase 3 of Restore Illinois, but Chicago is going to lag behind. Can I go to the beach? Can I go visit my brother? Should I make plans for summer vacation? As you can guess, there is no one right answer. It stinks, because I’d like to be definitive one way or another for you, but I can’t. What I can tell you is that you will only be completely safe if you stay in your home, eat out of your garden and come into contact with no one until there’s a vaccine that works. I don’t think that is a realistic or desirable option.
So, what do you do? Well, first of all, reach out. As a member of our practice, we want to help guide you through this process. I remember way back at the start of this on March 10th I made a strong recommendation to a septuagenarian to not travel internationally. Instead of being in the Middle East on March 12th, thankfully he and his wife were still in Chicago. If you recall, that was the infamous St. Patrick’s Day weekend in Chicago that triggered the mayor and governor to shut things down. I then wondered if he would have been safer in a remote location instead! It’s rare for me to make strong recommendations like that, as I do believe that individuals have the freedom to make choices for themselves as long as they understand the risks and benefits of a particular choice. So, how do we make such choices in a rapidly changing environment? It’s not easy.
As you make any decision—buying a car, having a surgery, hiking a mountain—there are risks and benefits to those decisions. For some, the risk is so low we don’t think twice, such as driving to the local Jewel. But what about driving Independence Pass in Colorado?

What is the problem we’re deciding upon? Well, in case you need a reminder, it’s COVID-19! COVID-19 is a viral infection mostly spread through close contact with infected people that causes an illness ranging from an asymptomatic infection to death. We now think that surfaces play a smaller role in transmitting infection. As you’re trying to make decisions about what to do and with whom, you need to first ask yourself, “How much do I care if I get this insidious virus disease?” If you really don’t care, then you can stop reading (and maybe reach out for a convo to discuss your thought process?). If you do care, then read on.
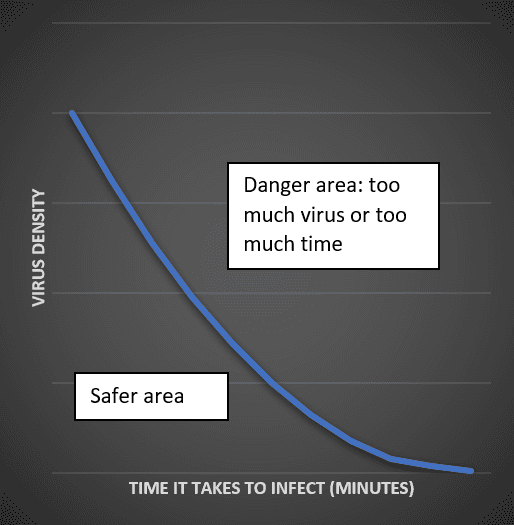
The risk of getting COVID-19 from an infected individual depends on how sick they are (their “virus burden”) and how much time they spend in your orbit. For even the sickest person, just passing them on the street or in a store likely isn’t enough. A good benchmark for “significant contact” is 15 minutes within six feet of you, mask or no mask, although the riskiest situation is if someone is really sick and you’re not wearing a mask. Here's a graph visualizing the risk, for those of you who appreciate this approach.
While the risk to children and young adults was thought to be very low, there are newer reports of cases of an inflammatory disorder that can be quite harmful. Also important to note, you can spread it to others before you know you have it. So, given the impact of the illness, the implications of our choices are that much greater. This isn’t a common cold we’re trying to avoid by skipping a luncheon in wintertime, or risking a sunburn by taking a walk without sunblock in the summer. You need to be comfortable with how much risk of getting this particular illness you are comfortable taking on.
What’s the next question? Who am I? No, this is not an existential question, it’s a question about your risk related to COVID-19. We know that the disorder can take anyone down, but there are certain factors specific to you (and those around you) that increase the chances of a more severe case of COVID-19. Here’s the list as provided by the CDC. If you don’t know whether you fit in one of these categories, ask us.
Moderate to severe asthma. Not mild intermittent, but moderate to severe.
Chronic kidney disease being treated with dialysis
Chronic lung disease such as COPD, emphysema pulmonary fibrosis, cystic fibrosis
Diabetes, Type 1, Type 2, gestational, MODY, etc. Any type of diabetes seems to be a risk
Hemoglobin disorders such as sickle cell disease or thalassemia
Immune compromised: Cancer, bone marrow transplant, solid organ transplant, stem cells for cancer treatment, genetic immune deficiencies, HIV, use of oral or intravenous corticosteroids or other medicines called immunosuppressants that lower the body’s ability to fight some infections (e.g., mycophenolate, sirolimus, cyclosporine, tacrolimus, etanercept, rituximab)
Liver disease including cirrhosis
People aged 65 and older: 8 out of 10 deaths in the US have been in folks over the age of 65
People who live in long-term care facilities like nursing homes
Serious heart conditions: heart failure, coronary artery disease, congenital heart disease, cardiomyopathies, and pulmonary hypertension
Severe obesity, meaning a BMI over 40.
So, once you get a sense of your risk, you then need to ask about the situational risk you’ll be putting yourself into. Is it worth doing? After not seeing family face to face for months, the answer for many may be a strong yes. If there’s a medical problem that you’ve delayed addressing, then the answer could be, “Now’s the time.” Yet if it’s, “I just need to get out. I’m going to eat at that neighborhood restaurant that has decided to open.” Would this be wise?
The moment you step out of your home you are adding to your risk. Your zip code is one key factor to assess your risk. The risk in Champaign, IL is lower than that in Chicago simply because there are fewer people walking around with the illness that you may encounter. One of our patients has been considering moving to another country. That country has a significantly lower rate of infection than Chicago, and their case tracking is much more advanced as well. It’s probably safer to be there than here (we address travel risk below).
Not only is your location important, but so is who you plan to be with. The greater the number of people you share your six-foot space with, the more risk you take on. This is why you see limitations on group sizes. What if the size of the group is o.k.? Do you know who's been in their pod? Do they even have one?
What about visiting other family that has been cooped up? Think about whether you want to absorb these people into your “pod”. Have they been isolating as well as you? Has their orbit been clear of dangerous satellites? If so, perhaps you can see them now before their circle gets opened up more and more. Now might be the time to see them with appropriate precautions, before they open their own circle and the risk goes up again. Once they’ve been with some friends who have been with some friends, it’s back to roulette. Don’t make the bet.
There’s been a lot of talk about religious services. Yes, I believe our faith traditions are essential, but should the expression of that faith put us at risk? My church is still working on plans and hasn't opened their doors to in-person worship. We need to allow the public health experts to take the lead on this. If they assess that is safer to begin to congregate in limited groups of non-pod members, then that should be our starting point. At the end of the week Illinois (except Chicago) will move into Phase 3 where groups of 10 are allowed. Could this be in a religious context? I believe, yes, as long as we’re masked, maintaining social distancing and keeping to approved group sizes. You can come in with your “pod” but don’t spend time in close proximity to others’ pods. If you can’t, then I wouldn’t feel it’s safe enough to begin to do that.
Some risk is much harder to control, though. I’ve had folks reach out with questions about air travel. Short flights are better, so think about that as you make plans. A few more variables to consider: how are you getting to the airport? If you can get a ride from someone in your “pod” that would be best. What about Uber or Lyft? Well, a big black SUV is probably safer because you can be further away from the driver. Keep the window open to allow for ventilation and the clearing of any virus cloud. Wear your mask as you begin your journey (surgical, KN95 or N95 if possible) and don’t touch anything. If you do touch something, wash your hands with hand sanitizer before touching your face.
Airports are apparently doing a better job with the lines at check-in, but be mindful of spacing and touching monitors. You’ll have more contact with items like bins as you go through security. Can you stick to the six-feet safety zone and clean hands rules as you move toward the gate? Possible. Do your best. While you wait at the gate, again keep your six-foot distance. Move around a bit. Don’t stay near anyone for a prolonged period of time. What about when you’re on the plane? First, continue to wear your mask. This is the most important time to be continuing to wear your mask. And while I personally prefer an aisle seat when I fly, these days I’d choose a window seat as there will be less contact with folks as they go down the aisle. I’d try and pick a seat in a row at the back of your section, whether it’s in First, Business or Coach. If you’re in the last row, you won’t have potentially infected people behind you who could express the virus toward you through a cough, sneeze, or animated conversation. What about the air on the planes? The air is circulated through filters that kill virus, so the fan above your seat is clean air. You can use that to disrupt the surrounding air. What you’re trying to avoid is the potential for the air of a nearby infected person to settle near you. Disrupt the cloud with the fan. Take your time getting off the plane. Don’t crowd in the aisle. Stay in your seat until the path is clear.
What about beaches and pools? The virus doesn't spread through water, so it's okay to swim. Again, it all comes down to group sizes and social distancing. Can this be maintained? Can you avoid being in close proximity to others on the pool deck and in the water? Being outside is safer, as the sun, heat, and breezes all contribute to the decreased risk. Nevertheless, masks on the pool deck (not in the water) and the six-foot rule are still advised.
Until there’s an effective vaccine or effective treatment, the safest approach is still to continue to limit your exposure to others. If you go out, wear a mask, keep your hands clean and social distance. Be safe!
Please let us know if you have any questions.
More to come,
Dr. Will
P.S. Our practice is accepting new patients. If you're reading, appreciate the content, and are not a member, please let us know if you'd like to talk with one of us about whether Harper Health may be right for you. In the age of telehealth and COVID-19, we have satisfied members all over the country.
Sign up below to join our newsletter